(Photo from Shutterstock)
- Obesity and diabetes rates in Mississippi are near the highest in the U.S.
In an effort to address the state’s obesity epidemic and subsequently address the health effects associated with it, the Mississippi Legislature is considering allowing GLP-1 medications such as Semaglutide to be covered under the state employee health insurance plan.
Currently, drugs that help people treat diabetes and/or address obesity are not covered under every health insurance plan, including the one offered to state employees.
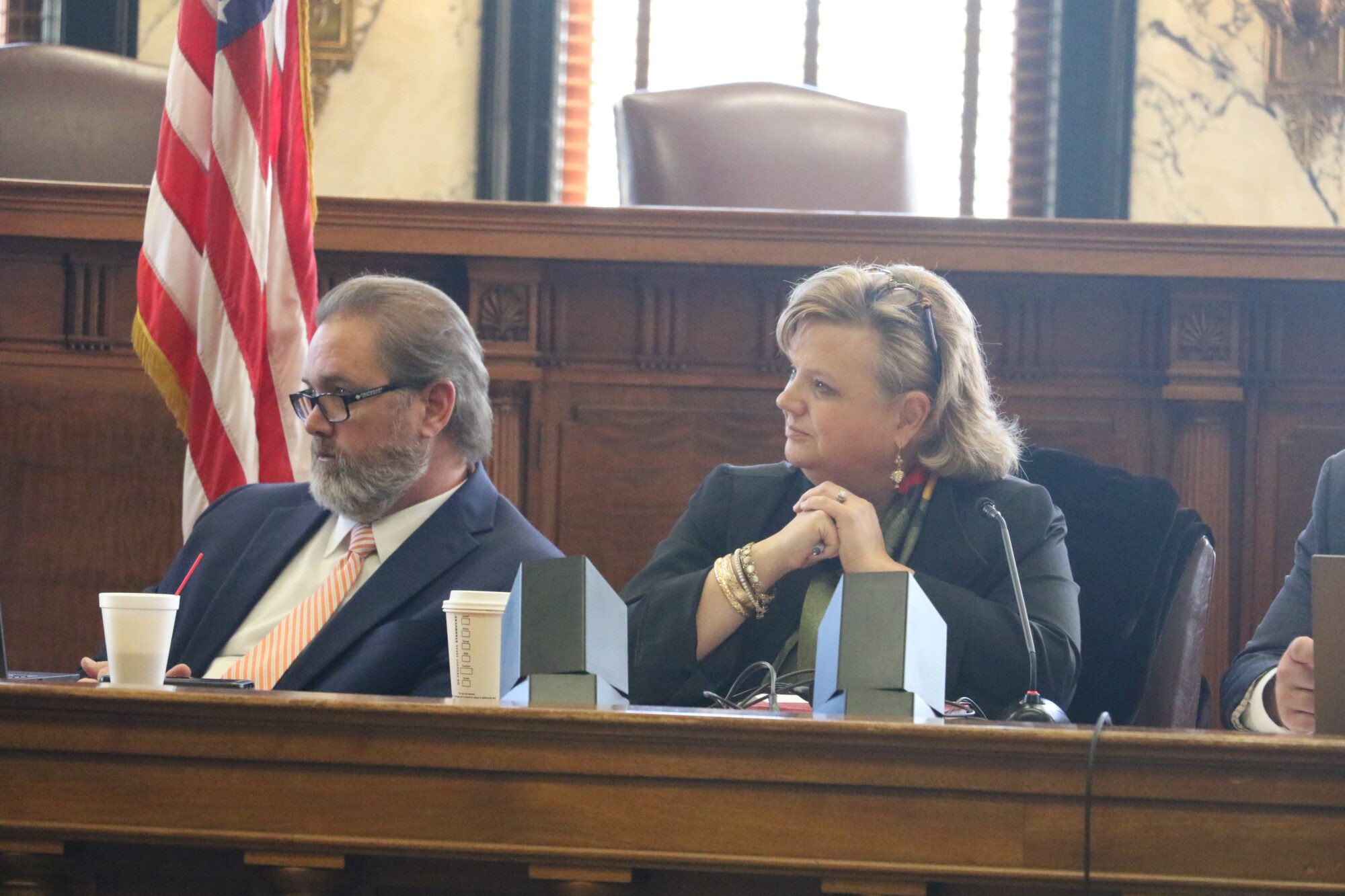
During the 2025 legislative session, SB 2401 was passed, forming the 11-member Insurance Study Committee. It is comprised of lawmakers, health professionals, and the state Insurance Commissioner, among others. The committee is tasked with certifying health benefit plans and health care services, said committee chair State Senator Walter Michel (R), author of SB 2401. State Rep. Samuel Creekmore (R) was selected as vice chair.
One of the considerations being discussed by the committee is whether the state employee health insurance plan should cover GLP-1 semaglutide medications. These drugs are used to manage diabetes or regulate appetite.
Brand names for those drugs include Ozempic, Rybelsus and Wegovy, among others.
Due to the drugs’ ability to allow a person to feel satisfied for longer after a meal, and their ability to control blood sugar, variations of semaglutide medications have demonstrated the ability to help people lose weight, said Dr. Courtney Walker. Walker is the Medical Account Director for Managed Markets with Norvo Nordisk, the company that manufactures Ozempic.
Walker said Mississippi is ranked second in the nation in obesity and diabetes rates. He also explained how obesity cases lead to diabetes and cardio metabolic diseases that increase co-morbidities. Those health impacts not only affect the patient in the short term but lead to increasingly expensive health care as the underlying health issues go untreated.
“It’s basically a firestorm of other diseases that can be impacted that ultimately can lead to heart and attack and stroke,” Walker described.
GLP-1 medications have also shown to be effective in treating inflammation of the liver, kidney disease, and high blood pressure, he added.
“What we know is that from 1999 until 2020, there’s been a threefold increase in obesity-related age-adjusted cardiovascular death,” Walker explained to the committee.
If changes are not made in the way Mississippians, and all Americans, look after their health, Walker said half of the nation’s population will be considered overweight or obese by 2030.
However, use of the drug is not guaranteed to influence a person’s body weight. Studies have shown, Courtney said, that one in three patients who took Semaglutide experienced a weight reduction of 20 percent. The drug achieves this by convincing the patient they are full faster. This could be advantageous since the societal norm is to lead sedentary lifestyles, while having more access to food.
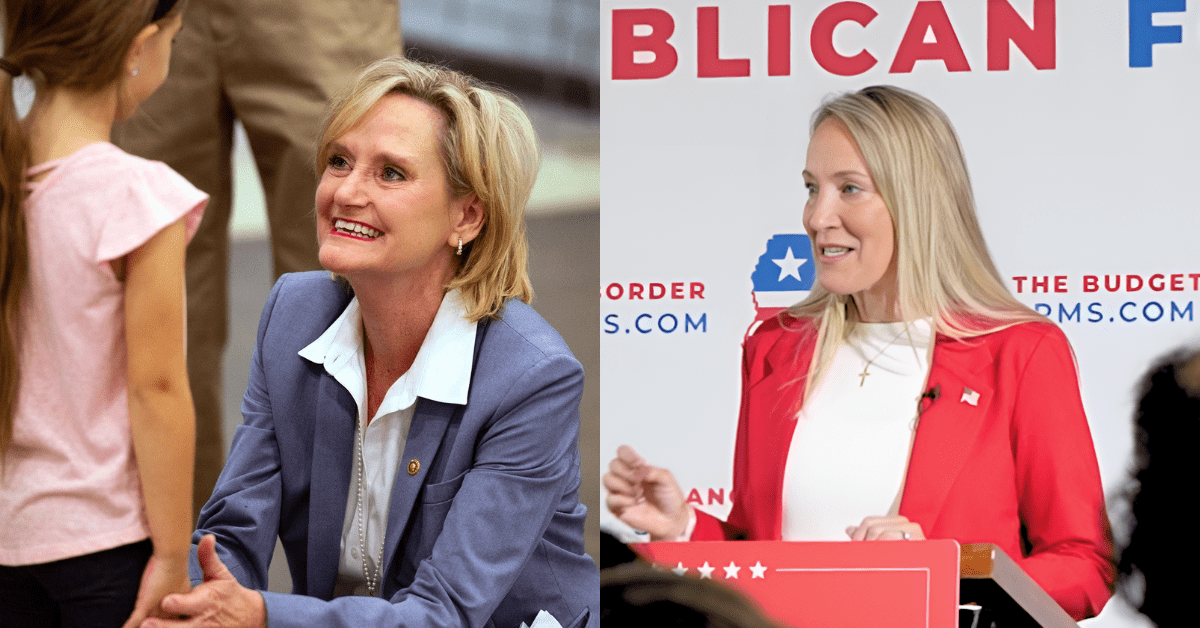
“But we also know that society has evolved,” said committee member Dr. Jennifer Bryan. “When you look at the big picture we sit at desks and at computer screens. We’re not raising barns like we were a century ago. We’re not burning calories the way we were. We’re not growing our own food and we’re buying in mass production.”
One of the problems with GLP-1 drugs is the expense, costing at least $1,000 for a month’s supply for those whose insurance does not cover the drug. Some manufacturers offer discounts for out-of-pocket purchases, Bryan said.
“If their plan does not cover it, the next choice is to pay $499, which we are grateful to the industry for coming down for that. It helped a category of people who can pay that much a month,” Bryan described. “But the average Mississippian cannot afford $500 per month.”
That cost would also be prohibitive to insurance plans if a large number of policy holders opted for a prescription, Bryan warned. She suggested starting with covering those who are at the highest risk until a generic version is available. One example of a high-risk patient Bryan told the committee was one with heart disease. Covering those patients at the highest risk could be a long-term cost savings over a couple of decades, especially since there are many risk factors associated with obesity.
“Obesity associated cancer is something a lot of people do not realize. Obesity is a huge driver of cancer,” Bryan described. “Just having something to combat obesity helps prevent downstream expense.”
Another option to lower the cost of the drugs could be compounded versions of the drugs, or versions made by a pharmacist using special formulations suited for each individual patient. The issue with those versions is they are not FDA approved because they have not been reviewed by the agency for safety.
State Rep. Creekmore said that discussions of trying to loosen those restrictions on compounded versions of the medication have not occurred yet, but the topic is something to consider.
“Especially if we’re considering this for the state health plan,” Creekmore told Magnolia Tribune.