- As the state evaluates how to improve rural healthcare, Bigger Pie Forum suggests policymakers consider all impacts – including the burden of skyrocketing PERS costs – on Mississippi rural hospitals.
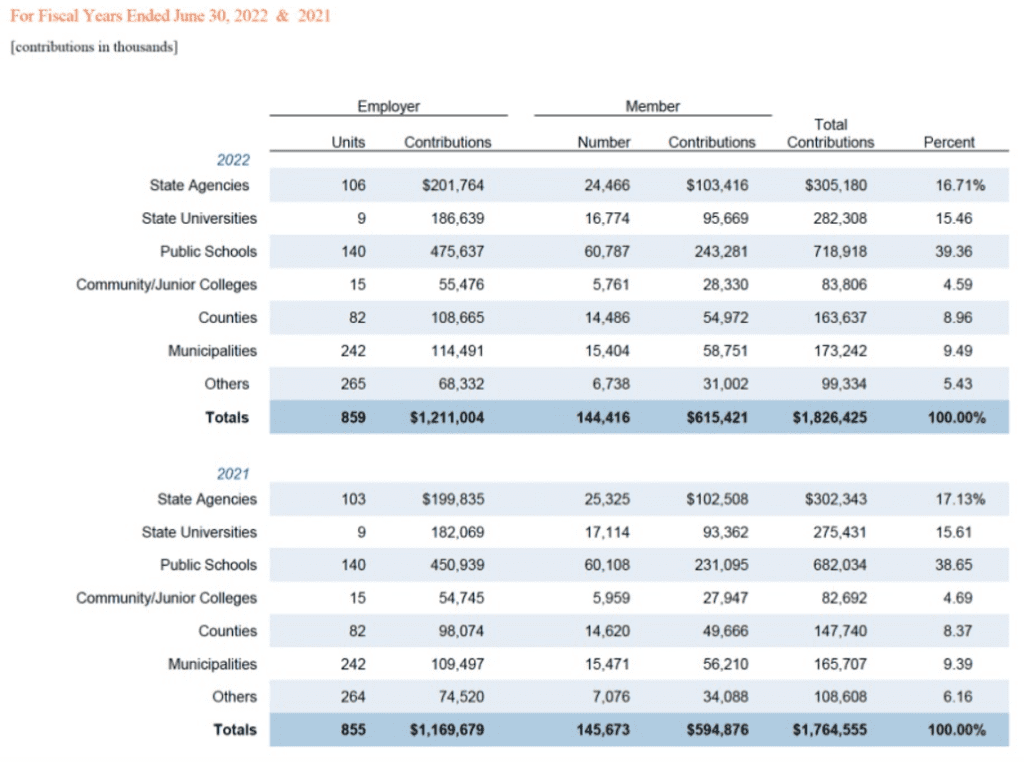
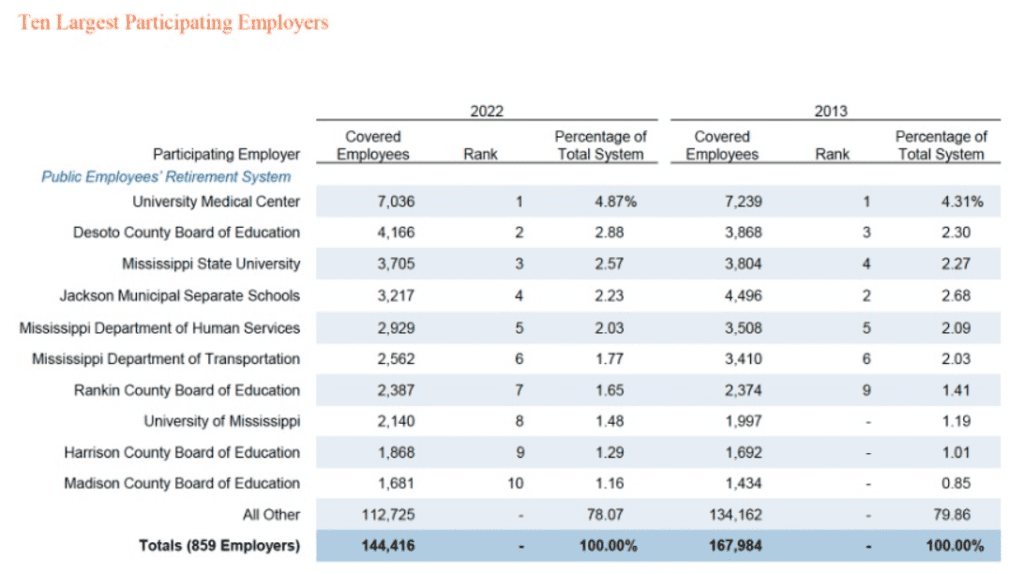
Did you know that PERS, the state’s retirement system, covers more than just state employees? In fact, the system covers employees of state agencies, state universities and community colleges, public school districts, cities and counties, and other entities like libraries, tourism bureaus, economic development districts, and even government-owned hospitals.
The 2022 PERS comprehensive report lists covered employers, including eight local hospitals in Port Gibson, Centreville, Meadville, Fayette, Corinth, Ruleville, Indianola, and Ripley. It’s hard to get more rural than the areas represented by these systems.
In fact, half of the covered hospitals are known as “Critical Access Hospitals” (CAH), a designation given to eligible rural hospitals by the federal Centers for Medicare & Medicaid Services (CMS). The Mississippi Department of Health recently noted our state’s critical access hospitals generally rank low compared to national averages, having negative total margins (-3.12 MS vs. 1.61 USA); negative cash flow (-0.36 MS vs. 5.71 USA); negative operating margins (-4.80 MS vs. 0.17 USA); and just 19.5 days cash compared to 75.9 days nationally. In the same report, the Department of Health highlighted shifts in CAH infrastructure, including skyrocketing demand for rural hospital services and increasing staffing challenges (more part-time workers and fewers LPNs and RNs).
It’s no secret that Mississippi’s rural healthcare system is struggling. A recent analysis suggests that some 30% of rural hospitals in our state are at risk of immediate closure; another report found that “small rural hospitals are being forced to close because they are not paid enough to cover the cost of delivering care to patients in rural areas.” An estimated 63% of rural hospitals lose money on services provided.
How does PERS impact this challenging healthcare landscape?
Let’s take a quick look at the PERS-covered hospitals. A 2019 Navigant report listed five of the eight as “at-risk hospitals” in an analysis of rural hospitals. And individual data from the CMS suggests continued financial challenges, particularly in patient services margins (3-year):
- Claiborne County Medical Center: -20.5%
- Field Health System: -10.3%
- Franklin County Memorial: -4.1%
- Jefferson County Hospital: -14.8%
- South Sunflower County: -3.9%
- Tippah County Hospital: -7.6%
Two systems, Magnolia Regional Health Center and North Sunflower Medical Center, had positive margins (16.5% and 21.6%, respectively).
A more recent report from the Center for Medicaid and Medicare Services (CMS) shows a similar four-year trend, with a significant increase in losses from 2021 to 2022 for all but two of the covered hospitals, as shown in Table 1.

Already, these hospitals face tremendous financial challenges in providing healthcare to rural Mississippians. Yet, rising pension costs places additional money challenges on systems.
Because these systems are part of the state retirement system, they are required to pay rising costs associated with PERS rate hikes. When the PERS Board votes to increase the so-called “employer” (i.e., taxpayer) contribution, that means higher costs for hospitals – with no end in sight. Since 1990, the taxpayer (hospital) contribution rate has increased eight times, while the employee (those who benefit from PERS) rate increased twice.
In 2022, there were 265 employers (including hospitals) that paid over $68 million in contributions. That’s an average of nearly $260,000 from the “employer” (i.e. taxpayer). Instead of investing that money in providing healthcare, these eight hospitals must redirect funds to pay for a pension system whose costs show no sign of slowing.
We find these increases unsustainable for taxpayers in general, and for hospitals in particular. As the state evaluates how to improve rural healthcare, we suggest policymakers consider all impacts – including the burden of skyrocketing PERS costs – on rural hospitals.