New Mississippi Division of Medicaid director shares information with lawmakers, addresses concerns
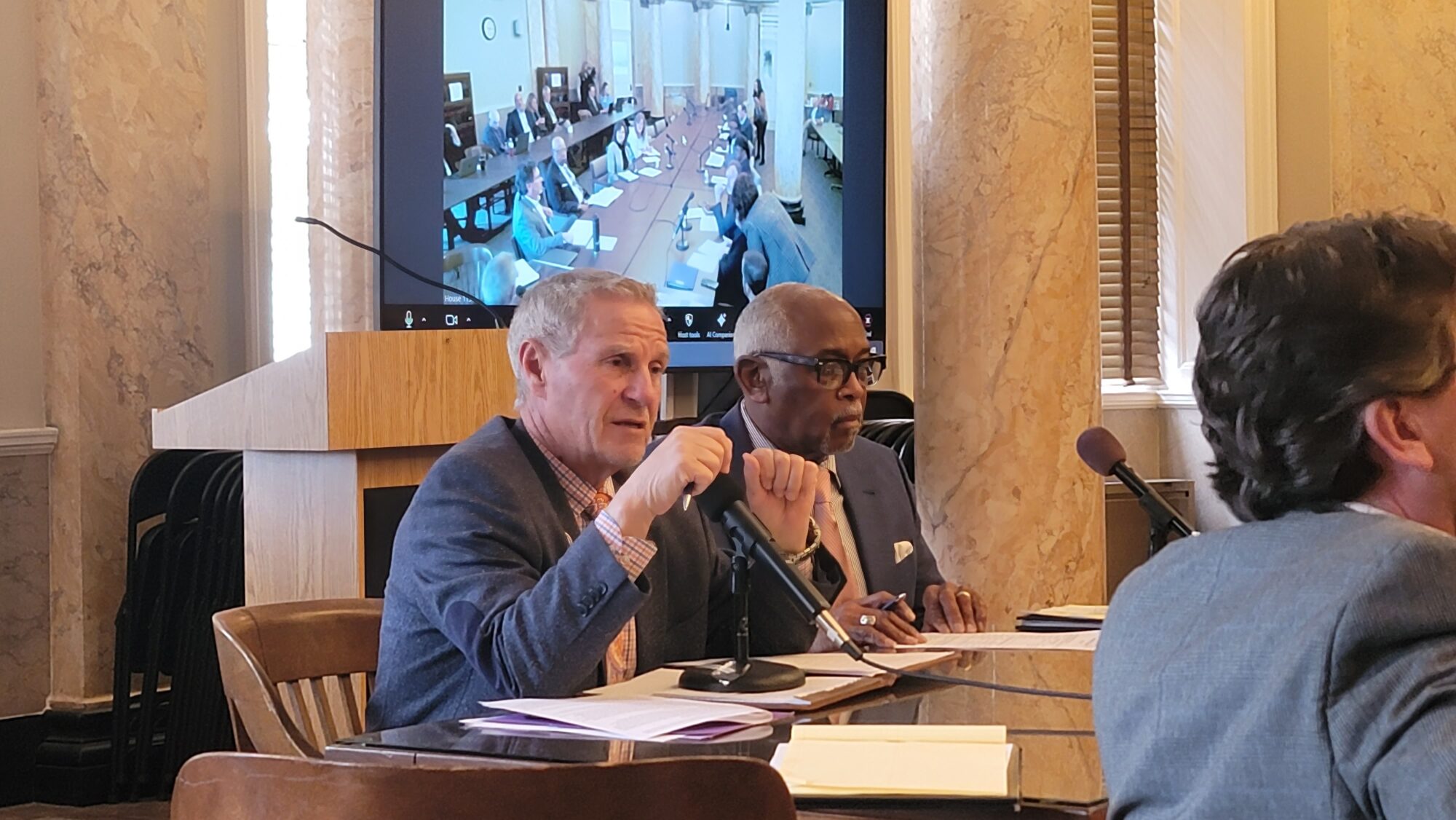
From left, House Investigate State Offices Chair Randy P. Boyd (R) and Senate Investigate State Offices Chair Albert Butler gather information about the current state of the Medicaid program in Mississippi during a meeting held Monday afternoon. Photo by Jeremy Pittari
- Mississippi Medicaid’s budget topped $8 billion this year, with nearly a billion coming from direct state support for the over 700,000 enrollees.
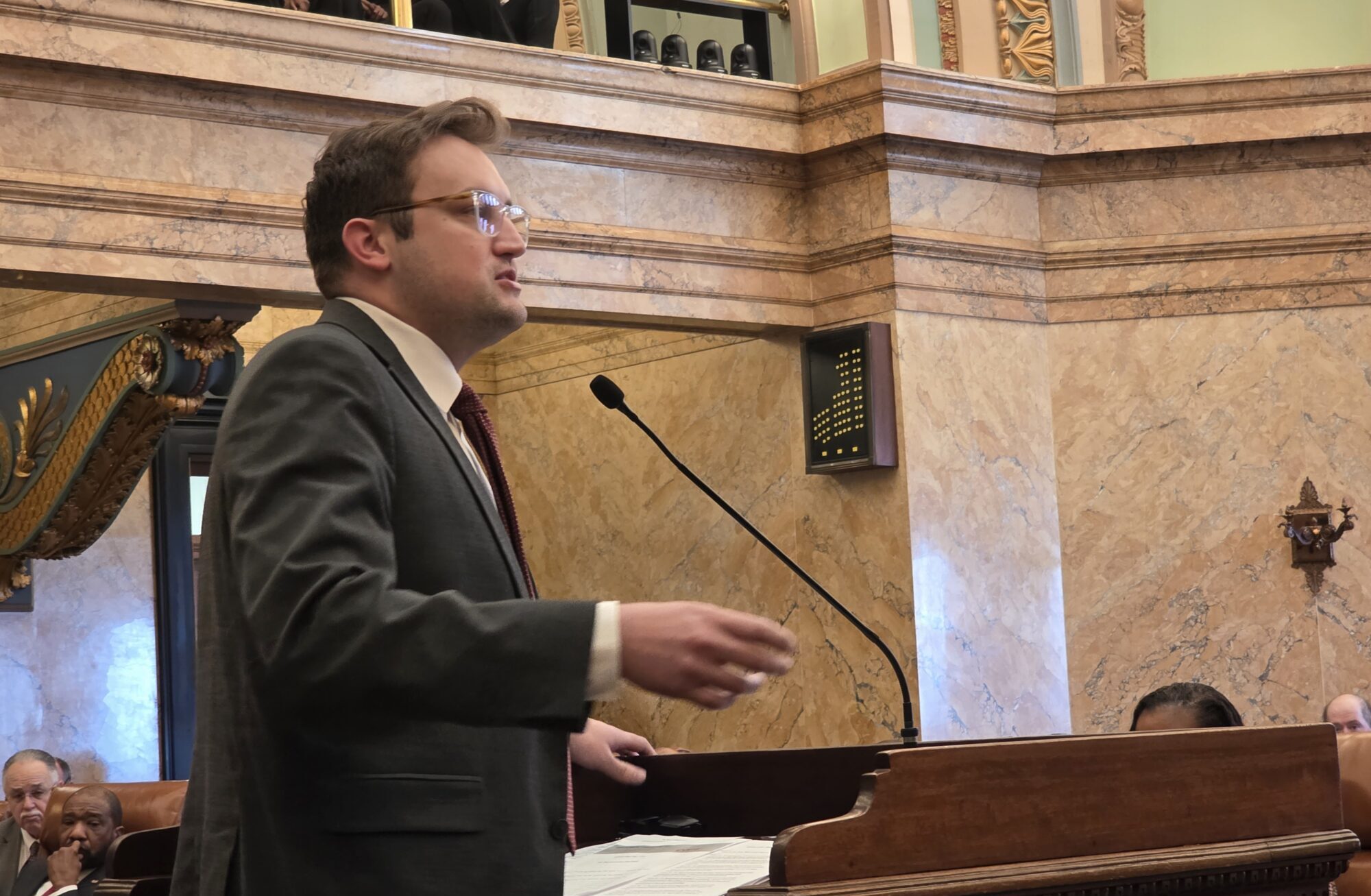
Lawmakers heard from new Mississippi Division of Medicaid Executive Director Cindy Bradshaw on Monday in a joint legislative meeting with House and Senate members.
Governor Tate Reeves appointed Bradshaw to the post in October 2024 following the resignation of longtime executive director Drew Snyder. Snyder is now a Deputy Administrator and Director of the Center for Medicaid and CHIP Services for the Trump Administration.
Bradshaw told legislators that within Mississippi, the Federal Medical Assistance Percentage (FMAP) is 76.9 percent, meaning the federal government pays the lion’s share of the public health insurance program for low-income persons. She said there is a possibility this percentage could drop in the coming years.
Mississippi’s current budget for the program is $8.1 billion, with the state’s direct support of $912 million.
Senator Kathy Chism (R) inquired as to how much the cost of Medicaid has increased in the state over the past five years.
“In the last five years, we were somewhere around $6 billion, and looking to 2025, we’re looking at somewhere around $8.1 billion,” said Jennifer Wentworth, Chief of Staff for the Mississippi Division of Medicaid.
Wentworth went on to say that the division expected the budget to increase to $9.9 billion in the next five years, but given the uncertainty at the federal level, she anticipated that would not be a good figure at this point.
Typically, a Medicaid recipient has to re-enroll every 12 months, but that process stopped for a time during the COVID pandemic. Bradshaw described how prior to COVID, enrollment in Mississippi was about 730,000, but during the pandemic the process to determine continued eligibility ceased.
“So, our rolls went up to about 904,000,” Bradshaw said.
Last year, the rolls were updated, leading to the current enrollment in Mississippi decreasing to roughly 707,000. Of that total, there are 107,000 Social Security recipients, 14,000 people in long-term care, 23,000 pregnant women, 315,000 children, and 10,000 children in foster care or in the custody of Child Protective Services.
With upwards of $800 billion in federal cuts to the Medicaid system being floated by Congress and the Trump Administration, Senator Joseph Seymour (R) asked how such cuts would affect the state’s program should they go into effect, especially if the state decided to expand the program as has been attempted in previous sessions.
“If it drops one percent, that’s about $83 million for a year for Medicaid’s budget that [the state] would have to come up with,” Bradshaw said. “If any cuts are made at the federal level, the state share’s going to go up.”
Mississippi’s Medicaid program utilizes three main vendors. Gainwell Technologies serves as the fiscal agent, processes fees for enrollment claims and service provider enrollment, among other services. Bradshaw added that it also acts as the data warehouse where reports can be pulled from claims. The other two vendors are Conduent, which oversees eligibility enrollment, and Telligen, that acts as the division’s utilization management.
There are also three managed care organizations that work with Mississippi’s Medicaid program: Magnolia Health, United Health Care, and Molina Healthcare of Mississippi.
Bradshaw told legislators that the Division of Medicaid now has less than a thousand employees.
Issues surrounding the Medicaid program
Concerns expressed about the Medicaid program include complications in the registration process and reimbursements are at times being clawed back as well as concern over the lack of pregnancy tests to determine presumptive eligibility.
State Rep. Randy Boyd (R) called attention to an issue with enrollment where people are reportedly being told by Magnolia Health that they do not work with Mississippi’s Medicaid Division, resulting in rejection notices. Bradshaw confirmed that there have been issues with some vendors having incorrect information and not processing terminations in a timely manner.
“That is something that we are working with them through currently,” Bradshaw added.
She told lawmaker that she has challenged all program areas to streamline processes to be more effective and efficient.
State Rep. Stacey Wilkes (R) asked why some providers are being challenged in their claims years after that a claim was approved and paid by the state, leading to the provider to have to pay a large bill. Wilkes said that the federal regulations would later determine that the care did not qualify, forcing the state to recollect previous payments years later.
Bradshaw said those situations typically occur when federal and state regulations do not align. One way to address it, she said, is to pay those claims through state dollars, but it would be expensive. Another way to shorten the confirmation time could come through updated software.
“That is something that really does bother me from a service standpoint and we are working on a couple of different ways to shorten that time period and do that more effectively,” Bradshaw described.
Senator Angela Hill (R) expressed concern about a lack of requirement to confirm pregnancy before presumptive eligibility is provided, such as through a pregnancy test. Bradshaw confirmed that on the federal level, providers are not allowed to ask for verification, so the House Bill currently being considered, HB 662, is proposing to make that change to abide by that federal law.
“This may sound crazy, but I feel like in today’s time I have to ask it, being that you can’t ask for a pregnancy check, is it possible that a man identifying as a woman can get presumptive eligibility if you can’t ask for pregnancy?” Hill asked.
Bradshaw admitted that could be the case. However, only OBGYNs and primary care physicians can provide presumptive eligibility approval, in addition to the health department. Essentially, she said, the program relies on providers to make that determination, and it is assumed that a pregnancy test is conducted.
Senator Hill suggested that in order to prevent fraud and abuse of the system that provision should be challenged and require a pregnancy test.