PBM reform bill passes in House, aims to bring down prescription costs

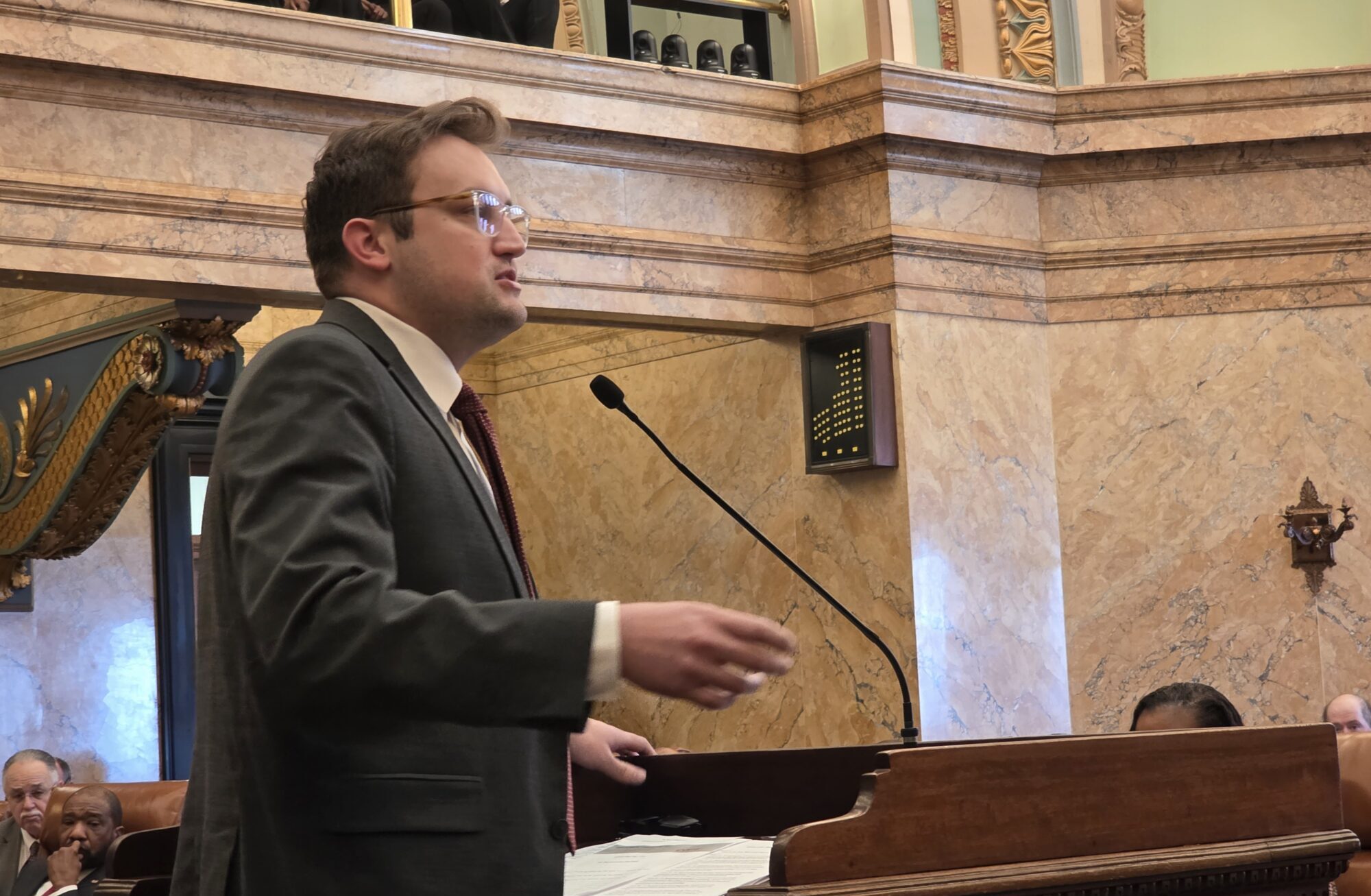
Rep. Hank Zuber describes HB 1665 on the floor of the House of Representatives during the 2026 legislative session. (Photo by Jeremy Pittari | Magnolia Tribune)
- “This is the only game in town, this is the only vehicle for PBM reform,” State Rep. Hank Zuber stated while explaining the bill to the House. “The Senate, for whatever reason, does not have a bill.”
The Mississippi House of Representatives passed a Pharmacy Benefit Manager reform bill on the floor last week.
The Pharmacy Benefit Prompt Pay Act, or HB 1665, is authored by State Rep. Hank Zuber (R). His stated goal is to remove clawbacks, ensuring independent pharmacists do not lose money when they fill prescriptions for medications. The measure would also place deadlines on PBMs to pay claims and do away with pharmacy steering and spread pricing.
There are currently no other bills being considered for the 2026 legislative session with the aim of PBM reform. The effort, advocates say, is intended to lower prescription costs.
“This is the only game in town, this is the only vehicle for PBM reform,” Zuber stated while explaining the bill to the House. “The Senate, for whatever reason, does not have a bill.”
Some of the provisions outlined in the legislation would mandate that the reimbursement cost provided to any pharmacist cannot be less than the cost incurred to acquire the medication.
“The independent pharmacists, if this bill passes, cannot be forced to fill a prescription for less than their independent costs,” Zuber told his colleagues.
The bill also creates a rule that electronic claims submitted by the pharmacist are to be paid by the PBM within 7 days, while written claims are to be paid within 35 days. Claims not paid in a timely manner would be subject to incur 1.5 percent interest per month on outstanding balances. Pharmacists also cannot be forced to pay through the plan if the patient prefers to use cash or credit card, and PBMs cannot employ clawbacks, which occur when a patient pays more for a drug when using credit as opposed to cash.
“You keep hearing about clawbacks. The PBMs are requiring the pharmacists to claw back some money. It stops the clawbacks,” Zuber said.
There will be no adjustments to the price at the point the claim was filed or when it is adjudicated, the Coast lawmaker added.
HB 1665 also seeks to create transparency by requiring all PBMs to publish claims and appellate processes on their websites, this could include contracts between PBMs and Pharmacy Services Administrative Organizations. Licensing for PBMs and PSAOs will be required, which would be subject to audits and financial statement requirements. They will also be restricted from charging more to a health plan than the drug actually costs, a process referred to as spread pricing.
“This bill completely stops spread pricing,” Zuber said. “It also requires all rebates to go back to the plan employer or sponsor, which will help all businesses.”
Under the bill, PBMs would lose the ability to steer patients to a particular pharmacy, such as one of their own, and they will be required to disclose if they own a pharmacy. The PBMs will also not be able to take retaliatory action against a pharmacist if a claim of wrongdoing is filed against the PBM.
“There’s penalties if that PBM tries to retaliate against that independent pharmacist,” Zuber explained.
Required reporting of the wholesale acquisition cost and retail cost of a medication is another aspect of the legislation.
Private and state plans would be forced to create a plan for specialty drugs, with the goal of opening more competition to make the prescriptions more affordable. Additionally, pharmaceutical contracts under state health plans would need to be re-bid every two years.
“I’m going to be blunt with you, very upfront. The money is made with the specialty drugs, that’s just the way of life,” Zuber said.
When asked by State Rep. Kevin Felsher (R) if the bill would lead PBMs to pass on the costs of meeting these requirements to the patients, Zuber said that opening up specialty drugs to competition is expected to lead to a decrease in costs.
“But that should be of concern, and that is something we thought about, what if the costs do go up?” Zuber responded.
To address any potential issues with the bill, it includes a three-year repealer, meaning lawmakers would relook at it in the coming years should it pass.
There is also a provision in the bill to ensure pharmacies affiliated with PBMs do not get lower drug prices than unaffiliated pharmacies, which typically include independent pharmacies.
Another provision of the legislation would expand the State Board of Health to include an independent pharmacist, a plan sponsor, and a Third-Party Administrator.
“And to me, that is a crucial part of this bill,” Zuber stated. “We are finally adding expertise and knowledge to the state health board.”
Enforcement and oversight of the provisions in the bill would be moved from the Board of Pharmacy to the Department of Insurance, he said.
The bill ultimately passed off the floor with a vote of 78-38. It has now been transmitted to the Senate for consideration.