The radiation and oncology entrance of the shuttered Charity Hospital building is seen in downtown New Orleans, Thursday, Nov. 9, 2017. Urban planning experts are about to make public their recommendations for the future of New Orleans' sprawling Charity Hospital. The 20-story, million-square-foot art deco building never reopened after levee failures during Hurricane Katrina caused catastrophic flooding in 2005. (AP Photo/Gerald Herbert)
- Unfortunately, Medicaid expansion in both states led to dramatic enrollment and cost overruns, while continuing to yield health outcomes that put Louisiana and Arkansas at the bottom of the heap nationally and failing to address risks to rural hospitals.
Comparisons between Mississippi, Louisiana and Arkansas are frequently drawn. The states share similar population demographics and many of the same historical education, economic and healthcare challenges.
Both Arkansas and Louisiana expanded Medicaid under the Affordable Care Act (commonly called Obamacare). So it’s no wonder their experiences are of interest to policymakers considering expansion here in Mississippi.
The goal of any healthcare related policy should be to improve health outcomes for citizens. Throwing billions of dollars at a problem might signal good intentions. But it is extremely costly window dressing if it does not yield the right outcomes. The measure of success for a program like Medicaid should not be how many people are on it, but how healthy the people on it are.
Unfortunately, both Louisiana and Arkansas are more “cautionary tale” than “success.”
What is Medicaid Expansion?
Medicaid was designed as a welfare program to help the most vulnerable people in society be able to access healthcare. Eligibility under the original program was limited to children, pregnant moms, caretakers with children, the disabled and the ederly. Because of low reimbursement rates, many physicians either do not accept Medicaid patients. Others limit the number of Medicaid patients they see.
When Obamacare passed in 2010, it sought to expand eligibility in two ways. First, it allowed able-bodied adults without dependents to become eligible for the first time. Second, it increased income limits for eligibility up to 138 percent of the federal poverty limit. After a court battle, the decision of whether to accept Obamacare’s expansion was left to the individual states.
Bigger Numbers, Higher Costs
In 2016, Louisiana’s Democratic Governor John Bel Edwards pushed Medicaid expansion. Health officials in Louisiana estimated there were 306,000 uninsured people in the Bayou State that would be added to the Medicaid rolls through expansion. The Louisiana Division of Medicaid’s latest annual report from 2022 reflects 638,000 people who have been added to Medicaid because of expansion.
| State | Estimated Expansion Enrollment | Actual Expansion Enrollment |
|---|---|---|
| Louisiana | 306,000 | 638,000 (108% above estimate) |
| Arkansas | 250,000 | 343,000 (37% above estimate) |
If you are doing the math at home, 638,000 is more than 306,000 — more than double, in fact. 44.5 percent of Louisiana’s population was on Medicaid at the time of the 2022 report. State and federal spending on Medicaid in Louisiana between 2016 and 2022 increased from $8.3 billion to $15 billion.
While Arkansas experienced less dramatic overruns in enrollment, the cost of the program ballooned at a similar rate. At its inception in 2014, Arkansas’s expansion was projected to add 250,000 uninsured enrollees. By 2022, the actual number of adults added was 343,000 — nearly 100,000 more than the estimate. Arkansas’s Medicaid budget went from $4.59 billion to over $9 billion in the same time period.
Same Bad Outcomes
Arkansas’s expansion has been in place for a decade. Louisiana’s, for almost 8 years. So surely their populations are much healthier, right? Unfortunately, no.
Despite the considerable expansion in both the number of people on Medicaid and the amount of money being spent, Arkansas and Louisiana’s health outcomes remain in line with Mississippi, near the bottom of the heap.
UnitedHealth Foundation publishes “America’s Health Rankings,” a report that looks at population health across the states using a wide variety of metrics. It’s a treasure trove of data that covers social and economic factors, physical environment, clinical care, behaviors, and health outcomes.
| State | Health Outcome Ranking | Overall Health Ranking |
|---|---|---|
| Mississippi | 46th | 49th |
| Lousiana | 48th | 50th |
| Arkansas | 50th | 48th |
The data suggest that health outcomes are not driven by access to Medicaid. A card in a wallet is not a cure. Cultural lifestyle differences across regions of this country appear to play a much larger role.
But at least Medicaid expansion stabilizes the decline of rural hospitals, right? After all, reports of hospitals at-risk in Mississippi have dominated political campaigns and media coverage over the last year. The one thing those reports have not done is to provide context outside of Mississippi.
The Center for Healthcare Quality and Payment Reform’s list of “rural hospitals at risk of closing” has been cited ad nauseam in support of Medicaid expansion in Mississippi. But this same source shows nearly the exact same percentage of at-risk rural hospitals in Louisiana and Arkansas:
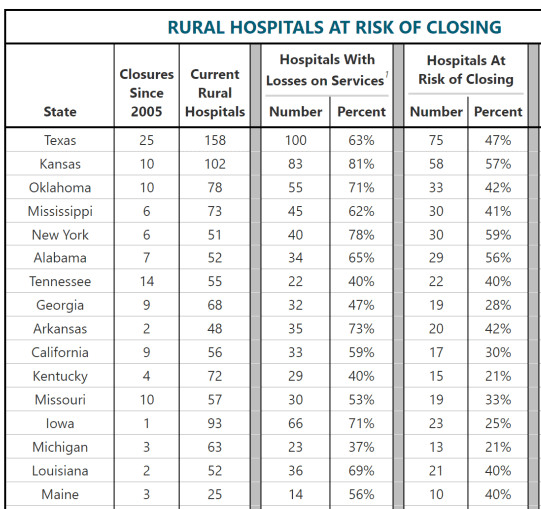
Notably, the list also demonstrates the volume of rural hospitals in Mississippi relative to most states, including states with far larger populations. On a per capita basis, only South Dakota and North Dakota have more hospital beds than Mississippi.
Becker Hospital Review published a list last year of 72 hospitals or hospital units that closed across the country. A considerable portion of these hospitals are in Medicaid expansion states.
Again, the evidence suggests there are more systemic issues afoot for rural hospitals. These include dramatically declining populations and a massive shift away from high-margin inpatient care that hospitals have historically relied on. Some of these pain points were exacerbated by COVID-era policies and inflation.