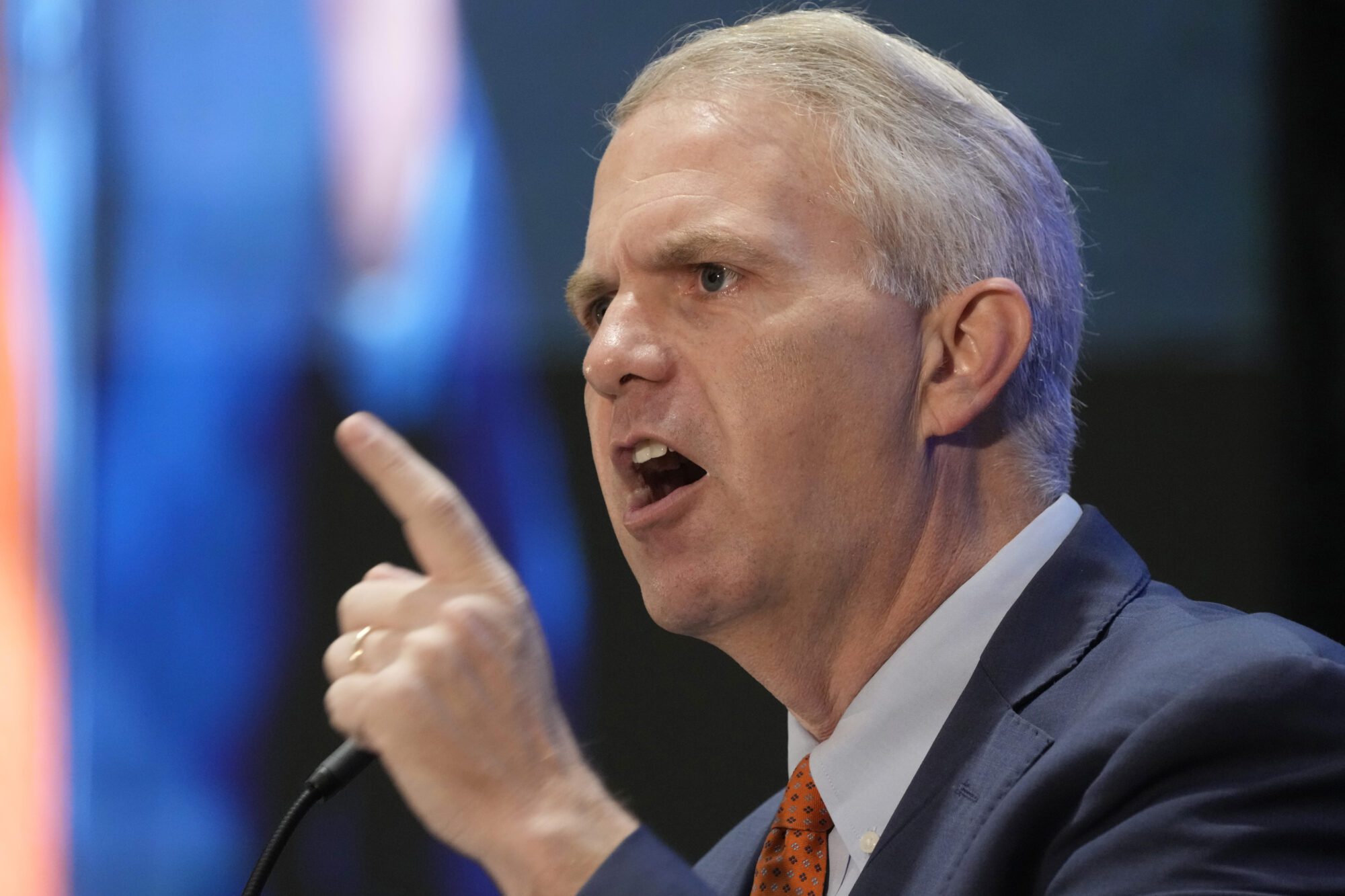
Drew Snyder, executive director of the Mississippi Division of Medicaid, gives members of the House of Representatives Medicaid Committee an outline of the state's Medicaid program at the Mississippi Capitol, Wednesday, Feb. 7, 2024, in Jackson, Miss. (AP Photo/Rogelio V. Solis)
- Medicaid Director Drew Snyder said the 9% uptick in state support is primarily due to federal match cuts. If expansion is considered, increases to state support will be even more.
The Mississippi Division of Medicaid (DOM) is requesting nearly $1 billion in state support moving into Fiscal Year 2025. The ask to lawmakers comes after nearly six years of no state support deficit since FY 2019.
Drew Snyder, Director of the Division of Medicaid, told members of the Senate Appropriations subcommittee on Tuesday that the decline in federal match for medical expenses was the primary driver of the requested increase.

The exact increased amount requested comes to $83 million, or an over 9% increase in state support. This surplus would help DOM avoid a deficit during the next fiscal year.
The FY 2024 request was approved at $909 million. The requested increase would put that number at $992 million, nearly $1 billion in state support.
DOM is also hoping to cover that amount with a portion of special funds from the Medical Care Fund in order to compensate for the non-federal share that does not have a state support impact.
Medicaid typically presents three request numbers to lawmakers within a fiscal year. There is an initial amount put forward in August, then again in January, and a final amount is presented in March when updated numbers from the beginning of the year can be calculated.
Snyder said the current number could change slightly by the third recommendation.
The DOM Director noted that the August 2023 number went up because the Federal Medicaid Assistance Percentage (FMAP) projected was lower than expected while utilization was higher than anticipated. He also indicated that this ask would not be the end of the increases.
While overall spending has gone up, state support spending has been flat for many years, after dropping $100 million since 2016. However, Snyder does not believe this will be a continued trend.
“We expect a dramatic increase in state support in Fiscal Year 2026,” said Snyder.
He said DOM expects to see continued annual drops in the federal share for the program. Those drops began in calendar year 2023. By FY 2026, Snyder estimated that the state support request could reach $1.449 billion.
Coupled with the declining federal funding percentage, Snyder said new federal policies on eligibility, potential utilization management restrictions and the continued rising labor costs mean the program will likely become more and more expensive to run.
Medicaid is funded by federal and state dollars. Based on FY 2024, the federal share for the state’s program came to $6.4 billion which include FMAP expenses, 50 percent of general administration costs, 75 percent of Quality Improvement Organization (QIO) expenses, 90 percent family planning, and 100 percent Indian Health Services.
The state support comes from special funds and general funds. That share historically covers most of the non-federal share costs and funds the Medicare Part D contribution of the “clawback.” In FY 2024 that amount came to $846 million.
When coupled with other state agency shares, provider taxes, the remaining cash balance and pharmacy drug rebates, the total non-federal share comes to $1.8 billion.
According to their graphs, DOM says the non-federal share burden for medical expenses is increasing 42 percent. This is largely due to the end of the COVID-19 public health emergency (PHE) 6.2 percent FMAP increase. Essentially, for every $1 sent on Medicaid the state was being required to put up 16 cents in 2023. By FY 2025, that will go up to 23 cents.
“The Medicaid program is going to cost substantially more to fund in the future and potentially fewer levers to control those costs,” said Snyder. “I do think despite those demands, success is possible.”
DOM was able mitigate the impact of the FMAP decline by using $682 million of their cash balance. Snyder said the remaining cushion will be used up by the end of FY 2025.
The yearly budget bill lawmakers consider sets the maximum that the DOM can spend in categories such as general funds, medical care fund, health care expenses and special source funds. This year lawmakers will also look at what is coined the “Medicaid Tech Bill” which outlines overall procedures of the DOM.
Prior Success of Medicaid
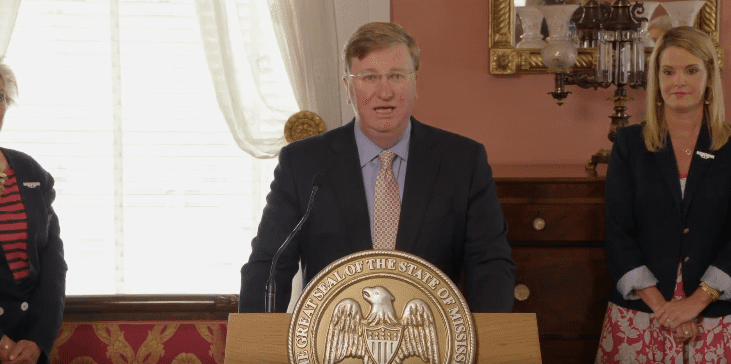
Despite concerns over the future of the program and what Snyder called a “balancing act” in ensuring its success, he said that 2023 was a positive year for the program. Data collected by the Division showed hospitals gained an additional $600 million after the CMS approval of Governor Tate Reeves’ reimbursement plan he announced last fall.
Other positives included the implementation of 12-month postpartum coverage care for pregnant women and member copays being eliminated. DOM were successful in the release of a member self-service portal, a new ambulance upper payment limit (UPL), and directed payment program.
“We actually received the best score in the country, in the percentage of women who have a delivery and have a time timely postpartum care visit,” said Snyder “That is a credit to our provider community and also our MCO’s.”
Medicaid funding was also able to provide hospitals with a one-time $137 million PHE-related payment.
For recipients, the continuous enrollment condition was eliminated and a new balanced approach which aims to make a more accurate re-determination and ensure continuity of coverage was adopted. Snyder said this change also protected taxpayers by immediately removing those who do not qualify for Medicaid.
Addressing talks of Medicaid Expansion
Enrollment in Medicaid peaked in the summer of 2023 at 904,000 with roughly 190,000 members being added from the beginning of the pandemic until 2023. Since the unwinding began, DOM is down 100,000 members but enrollment is expected to remain slightly above pre-pandemic levels. Currently, there are just over 800,000 people enrolled in Medicaid in Mississippi.
During the Senate committee hearing, State Senator Kevin Blackwell (R) recalled conversations among members to look at Medicaid expansion this year. He said many other states who have done so missed the mark when it came to estimating how many of their residents would be added to the rolls.
Experts estimate if Mississippi were to expand Medicaid, somewhere around 200,000 people could be added to the rolls. Based on what other state’s saw, Senator Blackwell said that was likely a low number and could be closer to 400,000.
Senator Blackwell asked Director Snyder what it would do to DOM’s budget if that decision was made. While he did not have exact numbers, Snyder said their research has shown gross costs could increase between $200 million and $250 million annually.
“It’s a pretty significant impact,” said Snyder. “Over time, that number is going to go up. You’ve seen how healthcare costs have been trending, $230 can become $300 quickly. The one thing we do know about Medicaid expansion projections is that they’ve all been proven wrong.”
If expansion is pursued, there is a 5 percent increase in the regular FMAP. However, Snyder said the cost for the federal match will go up and impact the state support amount.