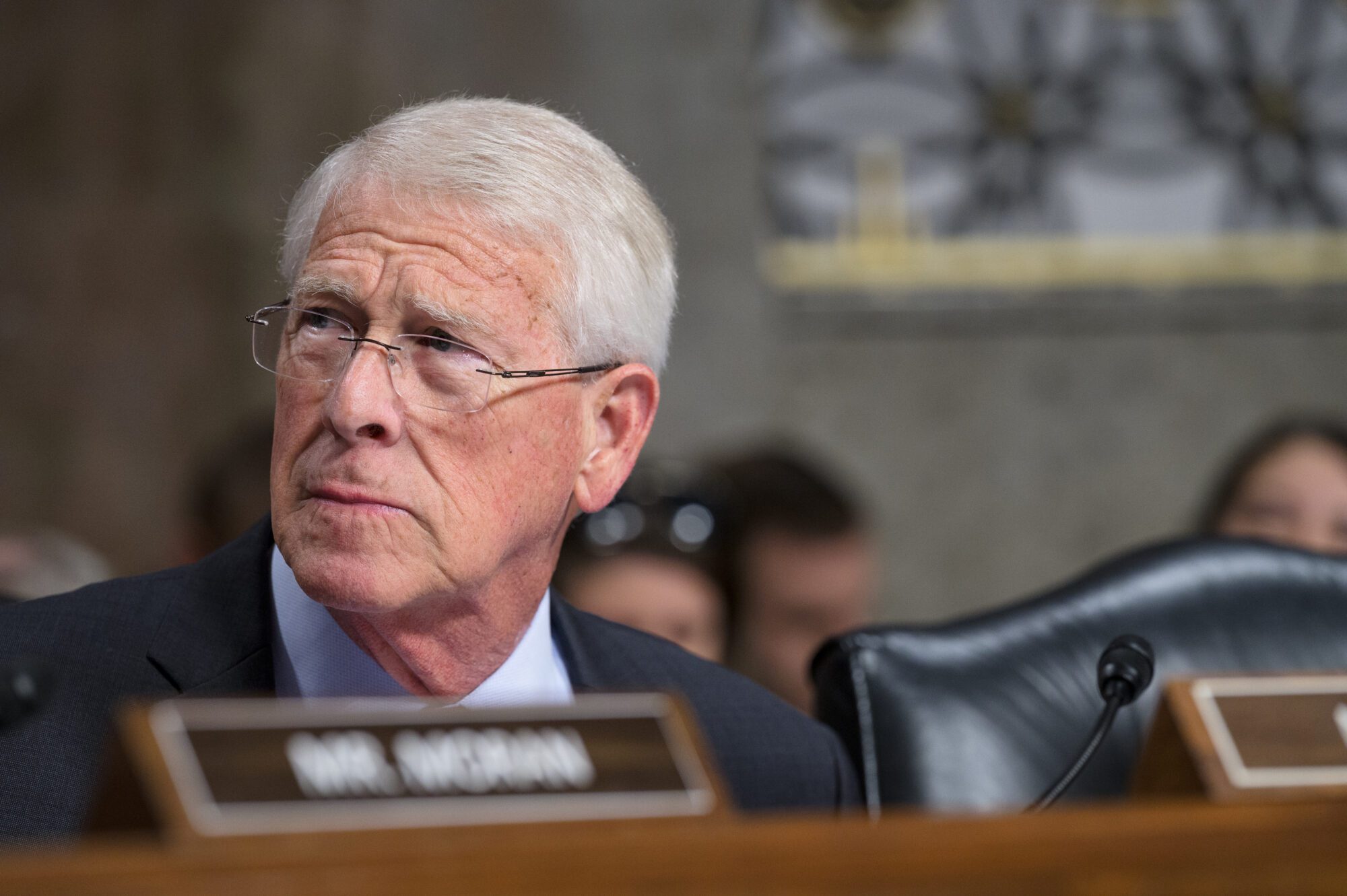
Legislators in the Mississippi House and Senate are continuing Medicaid hearings at the Capitol to prepare for the upcoming 2021 Legislative session. The Medicaid Technical Amendments bill is expected to be one of the largest items lawmakers tackle. The next round of hearings are to take place the week of Thanksgiving.
Just before the election, Legislators heard from more players involved in the application of Medicaid. The Mississippi Hospital Association kicked off the presentations on the first day. Tim Moore, MHA president, began his remarks by complimenting the Division of Medicaid staff who he said have been entirely different to work with under the direction of Drew Snyder.

Mississippi hospitals currently employ over 58,000 people, which represent 119,000 types of jobs and roughly $8 billion in wages.
It is no secret that Mississippi hospitals are in favor of expanding Medicaid. Just last year, hospitals had approximately $616 million in uncompensated care, a burden they estimate could be reduced by 40 to 50 percent if expansion were to occur. They expect hospitals will be funded around 2/3 of the state share that is needed for FY 2021.
In 2018, SB 2836, the Medicaid Bill, did help hospitals with these costs. It removed the five percent reduction for hospital outpatient payments and allowed for flexibility in supplemental payment models. The bill eliminated any cap on physician visits and prescription drugs for Medicaid recipients. It also increased reimbursements to OB-GYN’s to 100% of Medicare rate and some psychiatrist services were matched at that reimbursement, as well.
However, Moore said some items were authorized but not executed. So far, the cost based reimbursement option for small rural hospitals up to 101 percent for outpatient services hasn’t been implemented.
Many of the issues he pointed out surrounded Managed Care Operators. He also said the ability for MCOs to use alternative payment methods and incentives has not happened either.
MCOs are currently still not sharing data with providers, as was required in SB 2836. He added that the required annual audits of MCO providers to determine their financial benefit have not been utilized.
Through the continued utilization of MCOs, Moore said that Mississippi paid $1.6 billion more in premiums than were made to providers for medical payments in calendar year 2019. That same year, MCOs made roughly $300 million in admin fees even with the $616 million in uncompensated care hospitals took on.
Further, since FY 2011, the direct state appropriation has grown 24 percent and total Medicaid and CHIP enrollment has grown two percent.
He said while hospitals are working to improve quality of care, MCOs are focused on the bottom line.
Hospitals hope to see an expansion in Medicaid, as well as, the removal of the MCOs. Moore said these changes could help provide health care coverage for low-income working adults, extend eligibility for pregnant women and expedite the Medicaid appeals process.
In the event that the MCOs are reauthorized this year, the Hospital Association recommended that the Legislature standardize and expedite credentialing and clinical guidelines, require that they pay no less than the Medicaid rate, require Medicaid to reduce MCO admin fees before reducing provider payments (to the extent of federal law), and require that one of the MCOs be a non-profit provider sponsored health plan.
However, the Legislature nor the Department of Medicaid have indicated an appetite for Medicaid expansion this year. Governor Tate Reeves has also repeatedly expressed his opposition to expansion.
Y’all Politics attempted to reach out to MCO’s but were not able to secure a comment before press time.