House conferees on Medicaid expansion legislation in 2024 (Photo by Magnolia Tribune)
- Conferees signed off on an agreement minutes before the Monday night deadline.
Minutes before the 8 p.m. deadline on Monday, Medicaid expansion conferees for the Mississippi House and Senate signed off on a conference report for HB 1725, keeping the issue alive and setting up another round of voting that could come as early as Tuesday.
General bill conference reports were subject to a Monday night deadline.
According to State Senator Kevin Blackwell (R), chairman of the Senate Medicaid Committee, the latest proposal adopted in conference largely reflects the Senate’s original Medicaid expansion legislation, mandating that a work requirement be approved by the Centers for Medicare and Medicaid (CMS) before the services were expanded.
RELATED: Senate offers another Medicaid expansion proposal ahead of deadline
However, the Senate’s original plan only expanded up to 99 percent of the Federal Poverty Level (FPL) and left people earning between 100-138 percent of FPL on federally-subsidized private health insurance plans through the ACA exchange.
The compromise commits to full Medicaid expansion up to 138 percent, a position aligned with the Mississippi House’s original proposal. Individuals on or eligible for ACA exchange plans would remain on those plans, but they would be rolled under the division of Medicaid. The state would become responsible for bearing 10 percent of the cost of those plans.
Prior provisions that would have appealed a CMS denial of the work requirement were stricken from the filed conference report. Instead, lawmakers elected to direct that the state reapply for work requirement approval annually, by September 1, in the event CMS does not approve their initial request. There is no future date noted as to when the reapplication process should end.
The Senate also compromised with the House on its original 120-hour work requirement per month, decreasing the required hours to 100. As in previous iterations of the legislation, exceptions for this requirement include full-time students, guardians of children under the age of six, those deemed physically or mentally unable to meet outlined requirements, or a primary caregiver for a disabled child, spouse, parent. Eligibility verifications were also reduced from quarterly verifications to an annual verification.
The conference report also reflected a 1% additional annual license or privilege tax of the gross amount of premium receipts on insurance policies and contracts, which was not previously included in the legislation.
Medicaid expansion has been a hotly debated since the beginning of the 2024 legislative session when the House of Representatives first presented its bill.
Originally, the House moved to expand Medicaid up to 138% of the FPL with directions to require the Mississippi Division of Medicaid to obtain a work requirement waiver from CMS by the end of December. However, full Medicaid expansion was not contingent on approval of the work requirement. The House bill would have expanded the program whether or not the waiver was approved.
RELATED: Deadlock continues on possible Medicaid expansion
Through several rounds of back and forth between Senate and House Medicaid leaders, it became clear that the sticking point between the chambers was the work requirement. The Senate was insistent that any Medicaid expansion be contingent upon the prior approval of a work requirement.
House leadership and conferees did not immediately respond to a request for comment on the signed conference report.
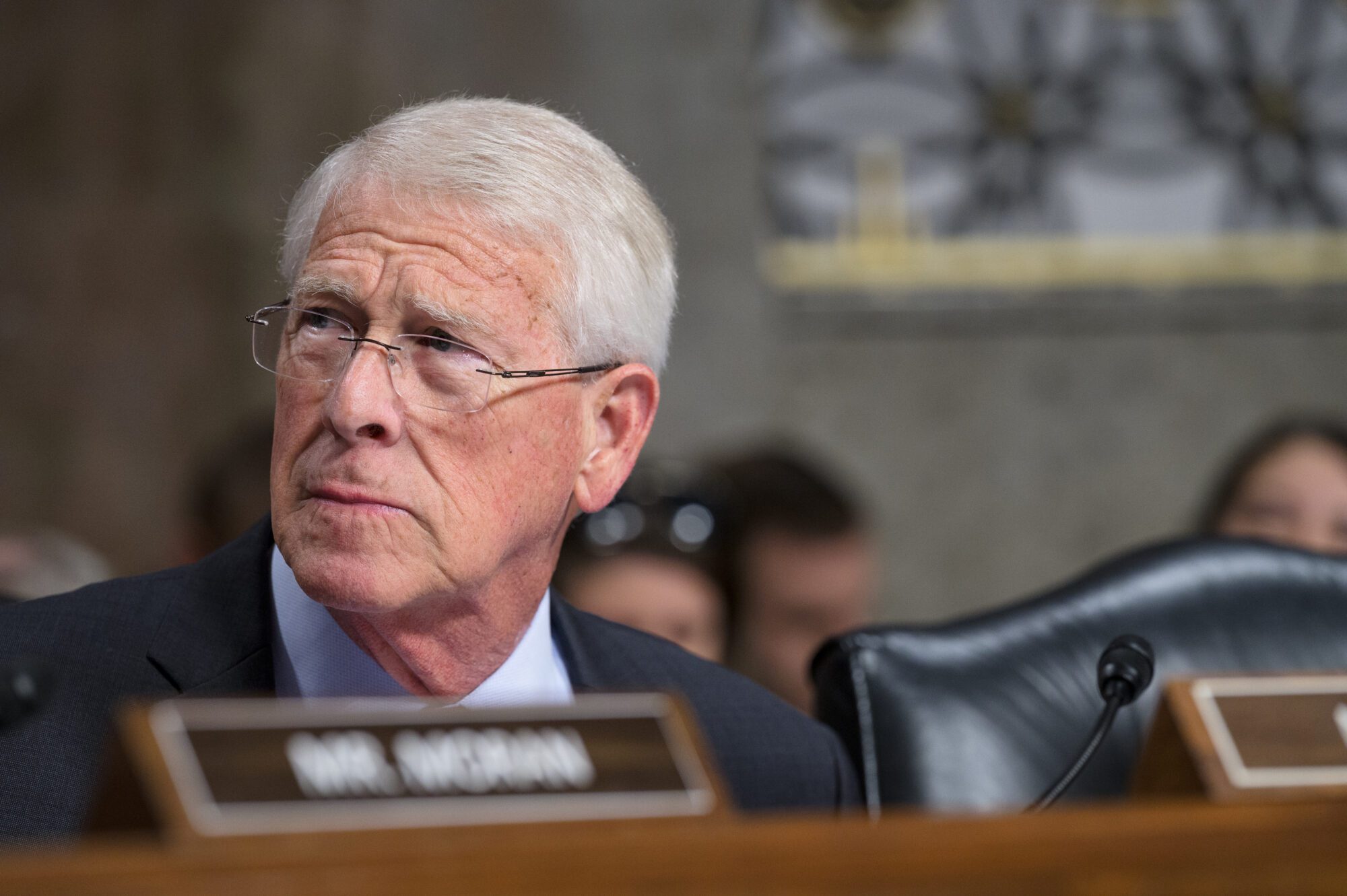
Governor Tate Reeves has openly communicated his intention to veto the legislation if it makes it to his desk, meaning the vote tallies, particularly in the Mississippi Senate, will be important.
Also now moving forward is legislation to institute a state exchange as well as the Medicaid tech bill which determines the parameters by which the Division of Medicaid is to operate. Currently, the tech bill that has been filed is a “dummy bill,” or a place holder, while additional details are finalized.