The Mississippi Division of Medicaid began to renew rolls in April and is expected to remove many who are not eligible for the program but received benefits due to COVID-era policies.
In March of 2020, Congress increased federal Medicaid payments to help states deal with the COVID outbreak. However, for states to receive the increased funding they were required to stop periodic eligibility reviews for enrollees.
This policy created what is known as “continuous coverage.” This meant, once someone was on Medicaid during that time period, they could not be removed, regardless of income level.
A sizable increase in Medicaid rolls resulted all across the nation.
In Mississippi, Medicaid rolls climbed from roughly 715,000 recipients at the beginning of the pandemic to over 900,000 recipients in May of this year.
In late May, the Congressional Budget Office estimated that 15.5 million people will be removed from the rolls over the next two years as states begin checking for eligibility, again. That’s roughly 20 percent of the 93 million Americans on Medicaid.
Brian Blase, president of Paragon Health Institute and former health care adviser to the Trump White House, told Magnolia Tribune that the increase in Mississippi Medicaid rolls was largely made up of people who are no longer eligible for the program.
“The sooner Mississippi does re-determinations to remove ineligible enrollees the more cost savings to the state,” said Blase. “The vast majority of people who are ineligible are enrolled in employer coverage, eligible for employer coverage, or eligible for a large subsidy to buy on the Obamacare exchanges.”
The Centers for Medicare and Medicaid Services (CMS), a government agency that oversees the health care programs, estimates $99 billion in improper Medicaid payments occurred in 2021.
Restoring Accuracy to the Rolls
In December of 2022, Congress passed the Consolidated Appropriations Act (CAA) which required states to begin redetermining eligibility of Medicaid members. As of April 1, Medicaid recipients were required to renew for eligibility. The federal government also began reversing its COVID-era increases in Medicaid payments in April.
In preparation for renewals, the Mississippi Division of Medicaid notified members to make sure all their contact information was correct. The re-determinations or renewals, must be initiated within 12 months and completed within 14 months.
According to the Division of Medicaid, it will take some time to know the impact of restoring eligibility requirements on the overall Medicaid population. During the renewal period, Medicaid is updating its numbers monthly.
At the end of May 2023, the Division of Medicaid reported 902,082 individuals on Medicaid. That breaks down to 454,673 children, 125,180 adults and 42,236 CHIP (Children’s Health Insurance Program) members.
The process consists of Medicaid working to renew a member’s benefits through an electronic verification source. If a member cannot be renewed electronically, Medicaid will send a pre-filled renewal form to that person. An individual will then have 30 days to respond with required income data.
States Seeing Enrollment Numbers Come Down
According to the Associated Press, more than one million people have been dropped from Medicaid since April. They say most of those individuals were dropped for not filling out the required paperwork.
Florida has seen the largest number of individuals removed from the Medicaid roll. The state saw a decrease of nearly 235,000 members from April to May. Other states with high numbers of removal include Arkansas, Idaho, Kansas, Nevada, New Hampshire, Oklahoma, South Dakota, Utah, and West Virginia.
Of the 15.5 million people who will lose Medicaid coverage as a result of restoring eligibility requirements, one in three already has private health insurance coverage.
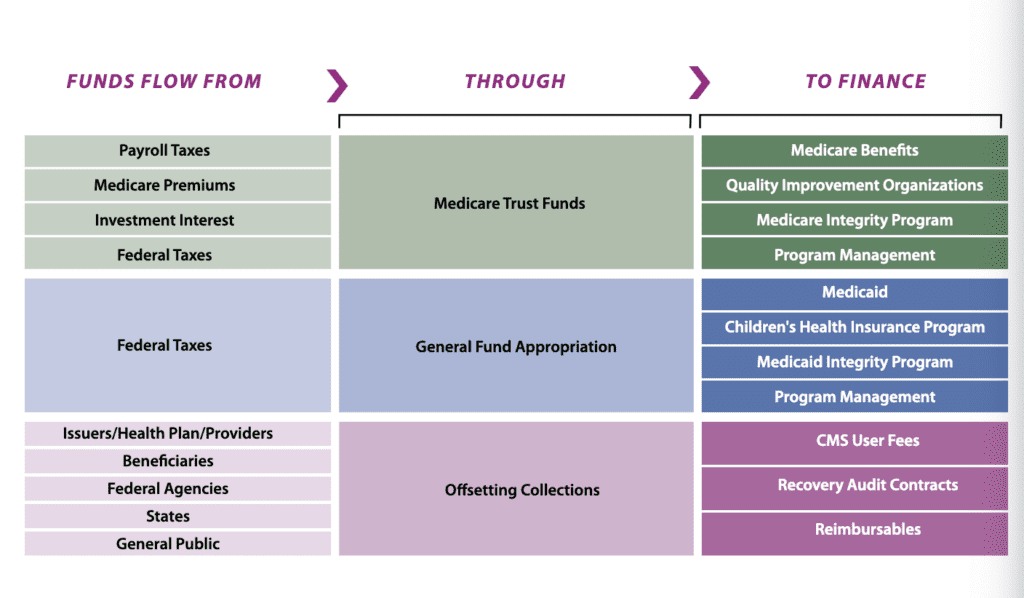
According to the Centers for Medicare and Medicaid Services (CMS), Medicaid receives financing from multiple avenues. CMS administers Medicare, Medicaid, CHIP, the federal Marketplace and the Clinical Laboratory Improvement Act of 1988 program. It is the single largest health payer in the U.S. It makes up more percentage of the market than private insurance providers.