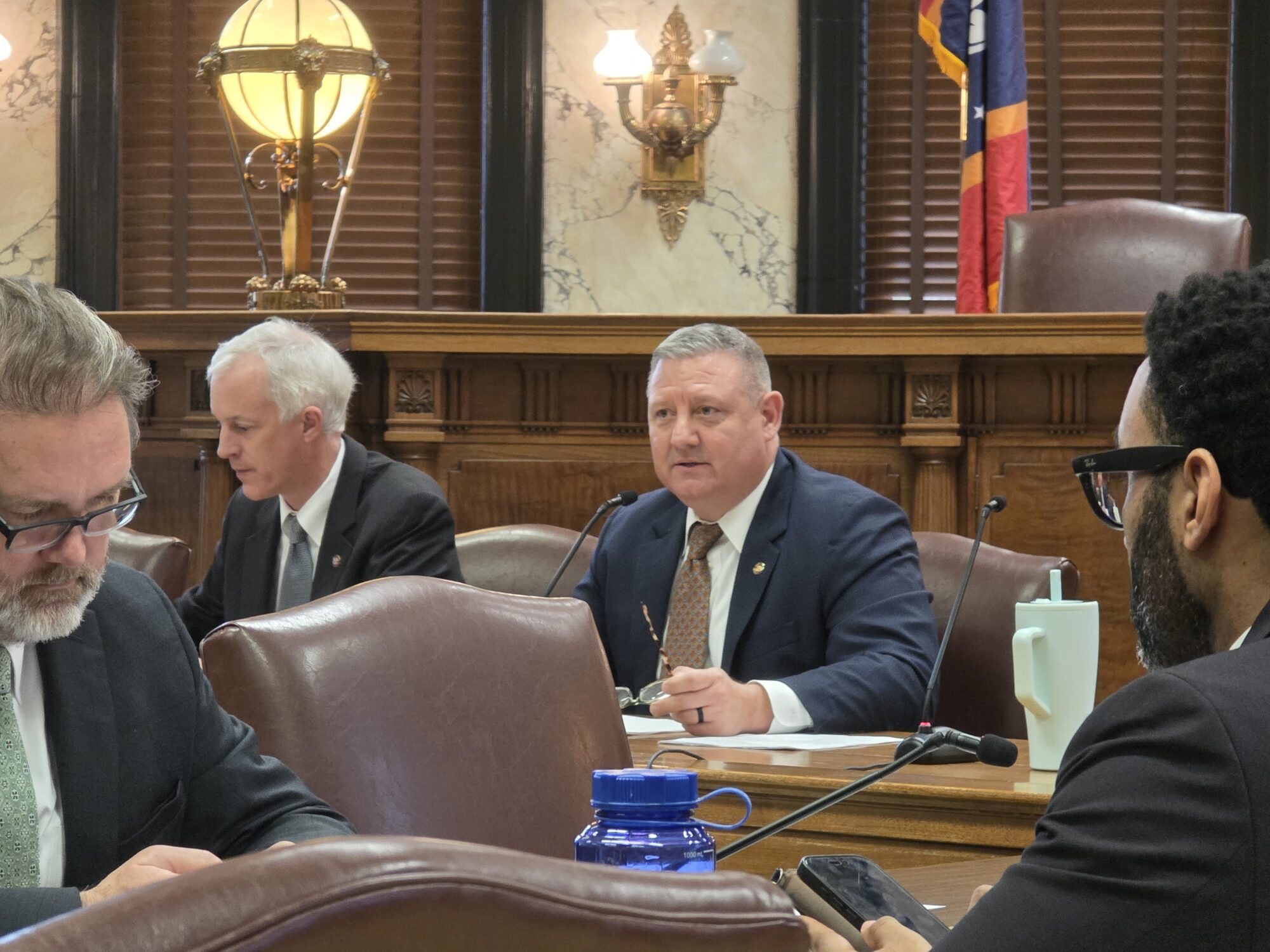
Moody: Medicaid tightening up on providers and recipients
Medicaid’s interim director, Bobby Moody, says the program is trying to “weed out the greedy” so it can take better care of the needy.
During an interview Wednesday with The Associated Press staff in Jackson, Moody said Medicaid workers are tightening up in two areas – on providers who bill too much for services and on patients who receive Medicaid benefits but aren’t eligible.
“Even though we lowered our rolls by a significant amount last year, we’re not hearing an outcry from members of the Legislature, we’re not hearing an outcry from the advocates out there that we’re kicking people off that are actually eligible for the services,” Moody said. “That speaks tons to me, that evidently we’re doing something right.”
Medicaid is a federal-state program providing health coverage for the needy, aged, blind and disabled and for low-income families with children.
In January, Medicaid started requiring recipients to do their annual reapplication for coverage in person rather than by mail. Applicants have to show proof of income and information about their living arrangements.
Moody said he believes the change in the enrollment process is responsible for the decrease of 20,113 recipients on the Medicaid rolls between June 30, 2004 and June 30, 2005. The program went from 768,004 recipients to 747,891 – the first enrollment drop in six years.
He said most ineligible people covered by Medicaid have simply been “no-shows” instead of trying to re-enroll. Based on the drop-off in the first six months, Moody estimated that the entire first year of face-to-face enrollment will trim about 50,000 people off the program.
Moody said when doctors, pharmacists or other Medicaid providers bill too much for services, the program first offers them a chance to explain what happened.
“If we’re comfortable that it was a clerical error, a billing mistake, then we recoup the money that we are entitled to recoup for the agency,” Moody said. “If we feel like there was some criminal intent, then we turn it over to the attorney general’s office or the (district attorney) in that area for prosecution.”
Some lawmakers and health advocates have criticized Gov. Haley Barbour for proposing cost-saving cuts in Medicaid. Changes in the program have to be approved by legislators.
At the Neshoba County Fair last month, three prominent Democrats – Attorney General Jim Hood, House Speaker Billy McCoy and former Gov. Ray Mabus – denounced Medicaid cuts.
“I don’t understand now why we’ve lowered Medicaid prescriptions from seven a month to five a month so we give some people a choice – you can either get the medicine you need to stay alive or you can buy the food you need,” Mabus said, talking about a change made this year.
Moody said he believes at least 90 percent of Medicaid recipients will receive all the prescriptions they need, even with the new limits.
For patients needing to stretch the coverage, Moody said he has the administrative authority to establish a “maintenance list” with certain drugs. Patients can receive a 90-day supply each time they refill a prescription from the list; the drug will count against a patient’s five-drug limit once every three months instead of once a month.
Moody served as a Democrat for 21 years in the state House of Representatives before Barbour tapped him to be a deputy director of Medicaid in May 2004. The former lawmaker became interim director of the program on July 1, after Dr. Warren Jones left the job.
“I think the perception that the governor is asking Medicaid to try to reduce the cost of state government on the backs of the poor is not correct,” Moody said Wednesday. “We are doing everything we possibly can to ensure that we provide the best service we can to a deserving population with the dollars we have available to us.”
Sun Herald
8/17/5