(AP Photo/Rogelio V. Solis)
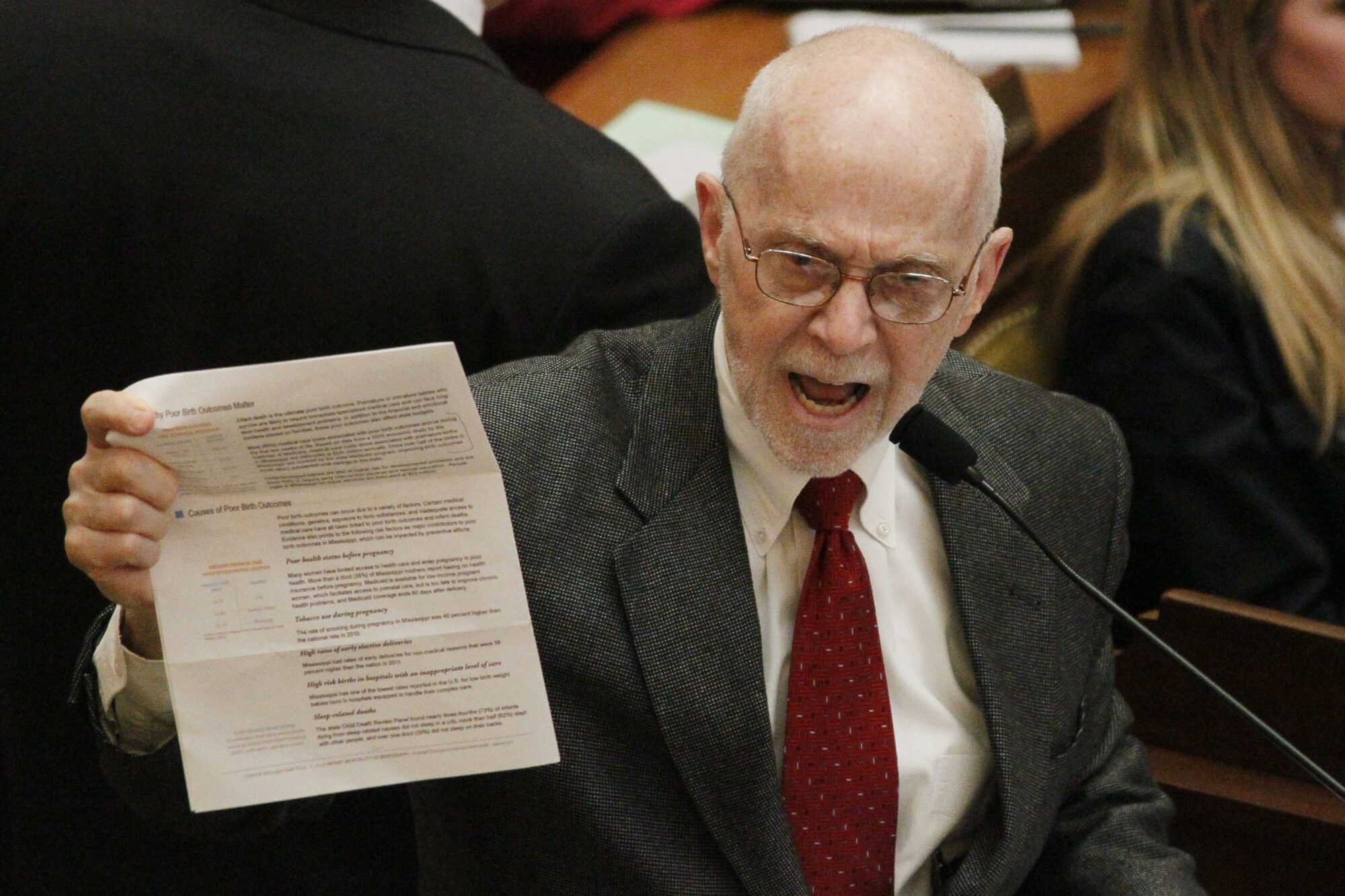
Division of Medicaid Executive Director Drew Snyder describes the proposal to change Medicaid reimbursement rates made by Gov. Tate Reeves, says there are four key advantages to the approach.
On September 21st, Governor Tate Reeves announced a series of Medicaid reimbursement reforms to bolster Mississippi’s health care infrastructure and better support hospitals throughout the state.
Once approved by the federal Centers for Medicare and Medicaid Services, these reimbursement reforms would generate nearly $700 million annually for hospitals.
Under the plan, hospitals would be reimbursed at Medicare rates for Medicaid fee-for-service patients and near the average commercial rate for Medicaid managed care patients.
Medicare rates for hospital services are higher than Medicaid. Commercial insurance rates vastly exceed both.
A recent Rand study estimated that commercial insurance rates for inpatient and outpatient hospital services in Mississippi were 193% of Medicare.
The Medicaid reimbursement reform plan announced by Governor Reeves is the most impactful action to help Mississippi hospitals right now.
The plan has several encouraging features besides the staggering net increase of $689 million dollars to hospitals.
First, the massive reimbursement hike for Mississippi hospitals won’t negatively impact Mississippi’s budget. A Medicaid plan to help hospitals today can’t threaten the sustainability of Medicaid program down the road. Instead of adding new recurring state expenses to the Medicaid program, this plan enables hospitals to draw down additional federal dollars for themselves through an already-existing state assessment on hospital beds.
Second, most of the funding is tied to the treatment of the over 800,000 Mississippians already enrolled in Medicaid. The largest component of the plan, a “directed payment” program, is required by federal law to be based on utilization and delivery of services.
Tying Medicaid payments to the treatment of Medicaid patients helps minimize politics, though the other component of the plan does preserve an option to assign a greater payment weight to small rural hospitals if needed.
Third, the plan builds on existing care quality initiatives. In recent years, Mississippi has used hospital directed payments to promote reductions in the number potentially preventable hospital admissions and potentially preventable complications.
More hospital funding through directed payments will place even more emphasis on the quality initiatives tied to the payments, and hopefully will lead to improvements in patient care.
Fourth, hospitals can receive the new funding relatively quickly. Payment processes are already in place and a substantial portion of the payments could be made within weeks of federal approval.
Medicaid was designed to serve the most vulnerable among us—seniors in need, individuals with disabilities, low-income pregnant women, and children. Better alignment between Medicaid rates and commercial rates in our hospitals helps avoid a two-tiered system: one for the most vulnerable and one for everybody else.
Anybody interested in the future of our hospital system has reason to be encouraged by policy developments this year. The legislature’s $103 million grant program, the $137 million one-time payment to hospitals in May, and now the new proposals announced in recent days are just some of the steps of an aggressive effort, in both the legislative and executive branches of government, to address the state’s hospital infrastructure.
The initial reaction to the planned reimbursement reforms has been extremely positive. Most of the negative feedback has come from people who have shown a propensity to oppose any solution that doesn’t include Medicaid expansion.
But at the end of day, thoughtful folks can disagree on whether to add working-age adults with zero income or income up to 138% of the federal poverty level to the Medicaid rolls, and still agree on the potential value of this latest approach to sustain hospitals.